Diag Image: The Future of Diagnostic Imaging
In today’s fast-advancing medical landscape, diag image plays a vital role in transforming the way healthcare professionals detect, diagnose, and treat diseases. Moreover, by combining modern medical imaging techniques such as X-ray, CT, MRI, and ultrasound with innovative AI analysis, diag image ensures faster and more accurate interpretations. As a result, this not only enhances clinical diagnostics but also supports doctors in delivering personalized care while reducing human error.
Furthermore, with the integration of machine learning models, diagnostic imaging is evolving into a more intelligent and reliable system, empowering hospitals and clinics worldwide. Consequently, as technology continues to improve, it is becoming the backbone of healthcare innovation, shaping the future of preventive care and precision medicine.
Table of Contents
-
What Does “Diag Image” Mean?
-
Major Modalities & Techniques
-
AI, Machine Learning & Deep Learning in Diag Image
-
Clinical Uses: Where Diag Image Shines
-
Implementation: How Healthcare Orgs Can Adopt Diag Image
-
Challenges & Considerations
-
Trends & Innovations
-
FAQs
What Does “Diag Image” Mean?
When people refer to diag image, they’re talking about the images produced by diagnostic imaging technologies—X-ray, CT, MRI, ultrasound, PET, and others—and all the supporting systems and workflows around them. However, in modern healthcare, “diag image” frequently implies more than just images capture. Instead, it includes image analysis, interpretation, AI assistance, and quantification of findings.
Key elements include:
-
Image acquisition (how the image is captured; manually or via devices)
-
Processing / image enhancement / noise reduction (to improve clarity)
-
Interpretation (by radiologists, physicians, or AI tools)
-
Integration with medical records, PACS (Picture Archiving & Communication Systems), RIS (Radiology Information Systems), etc.
Major Modalities & Techniques
Understanding the different modalities helps us appreciate what diag image can do. For example, each technique provides unique insights:
| Modality | What It Offers | Common Use Cases |
|---|---|---|
| X-ray | Fast, widely available; good for bones, chest, dental | Fractures, pneumonia, joint issues |
| Computed Tomography (CT) | Cross-sectional views; detailed bone + soft tissue contrast | Trauma, internal organs, vascular studies |
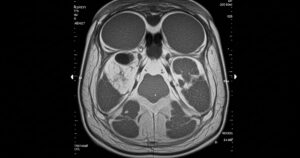
| Magnetic Resonance Imaging (MRI) | No ionizing radiation; high soft tissue contrast | Brain, spinal cord, muscle & ligament injuries, tumor detection |
| Ultrasound | Real-time, portable, radiation-free | Obstetrics, vascular imaging, guiding biopsies |
| Positron Emission Tomography (PET) | Displays metabolic/functional information | Cancer staging, recurrence, combining with CT or MRI |
| Mammography | Specialized for breast tissue imaging | Breast cancer screening / diagnosis |
AI, Machine Learning & Deep Learning in Diag Image
Modern this isn’t just about snapshots; instead, it’s about smart analysis.
-
Deep learning neural networks (especially CNNs) trained on large datasets can detect subtleties that may escape human eyes.
-
Moreover, machine learning models focused on specific conditions (like cancer detection, stroke, and cardiac anomalies) are becoming more accurate.
-
In addition, AI-assisted diagnostics now offer decision support: flagging anomalies, quantifying measurements, and estimating risk.
-
However, explainability and transparency are increasingly demanded. Clinicians want to know why an AI flagged something. Therefore, this helps build trust and manage liability.
Clinical Uses: Where Diag Image Shines
This adds impact across many specialties. For instance:
-
Oncology: early tumor detection via mammograms, lung CT, skin imaging; cancer grading using histopathology.
-
Neurology: stroke detection in emergencies, quantifying brain lesions in multiple sclerosis, tumor monitoring.
-
Cardiology: measuring ejection fraction, assessing coronary arteries, detecting heart disease.
-
Musculoskeletal & Orthopedics: identifying fractures, degeneration, tendon/ligament damage.
-
Emergency Medicine: rapid triage, detecting injuries, guiding interventions.
Implementation: How Healthcare Organizations Can Adopt Diag Image
Adopting it requires careful planning. Therefore, here are some best practices:
-
Needs assessment – Evaluate infrastructure, staff skills, workflows, PACS/RIS/EHR integration.
-
Pilot projects – For example, start with chest X-ray AI; measure KPIs like diagnosis speed and accuracy.
-
Workflow integration – Ensure tools complement existing systems rather than disrupt them.
-
Staff training & change management – In addition, provide clear communication on AI benefits and limits.
-
Validation & QA – Validate AI locally; monitor drift; manage false positives/negatives.
-
Security, compliance & regulations – Protect data, ensure approvals (FDA, CE), and meet privacy laws.
-
Cost & ROI analysis – Consequently, weigh costs (hardware, licensing, training) against benefits like reduced errors and faster diagnoses.

Challenges & Considerations
While diag image offers great promise, there are hurdles.
-
Algorithm bias: datasets lacking diversity reduce accuracy.
-
False positives/negatives: misclassification may lead to unnecessary or missed treatments.
-
Data privacy & security: sensitive images require strong protection.
-
Integration complexity: legacy systems and varying formats (DICOM, HL7) cause issues.
-
Costs & infrastructure: GPUs, storage, and networks add expense.
-
Regulatory & liability issues: Who is responsible if AI misses something? Therefore, approvals and safeguards are essential.
Trends & Innovations
The future of diag image is exciting. For example:
-
Federated learning & privacy-preserving AI: models trained across institutions without sharing raw data.
-
Multimodal AI: combining imaging with genetics, clinical history, and labs.
-
Edge computing & mobile imaging: diagnostics at the point of care.
-
Real-time/4D imaging & AR: assisting surgeons and remote consultations.
-
Explainable AI: confidence scores, heatmaps, and interpretable outputs.
FAQs
1. What accuracy can AI-powered diag image systems achieve compared to radiologists?
It depends on the task. For instance, AI often matches or slightly exceeds expert accuracy in specific cases. However, the best results usually come when AI augments radiologists rather than replacing them.
2. Are there risks with radiation exposure in diag image techniques like CT or X-ray?
Yes. However, modern protocols reduce exposure significantly. In contrast, MRI and ultrasound have no ionizing risk.
3. How do hospitals adopt diag image without disruption?
In general, start small: pilot projects, staff training, and gradual scaling ensure smoother adoption.
4. What infrastructure is required for diag image?
Hospitals need high-resolution imaging hardware, secure storage, fast networks, and AI-ready computing (like GPUs). Additionally, PACS/EHR integration is essential.
5. How do regulatory approvals work for diag image systems?
They vary by region. For example, in the U.S. FDA approval is required, while Europe uses CE marking. Therefore, validation and documentation are critical.
Conclusion
“Diag image” represents far more than pictures of the body; instead, it is a gateway to smarter, faster, and more precise healthcare. By combining modalities like CT, MRI, X-ray, ultrasound, and PET with AI, machine learning, and strong infrastructure, healthcare systems can improve diagnostics, reduce errors, and save lives.
Consequently, for hospitals, radiology departments, and health tech leaders, now is the time to invest in diag image solutions. In the end, the organizations that lead adoption will deliver better outcomes, improve efficiency, and lower long-term costs.



